| Influenza A virus | |
|---|---|

| |
| Structure of influenza A virus | |
| |
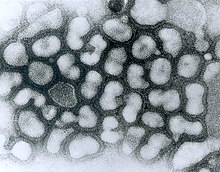
| TEM micrograph of influenza A viruses | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Insthoviricetes |
| Order: | Articulavirales |
| Family: | Orthomyxoviridae |
| Genus: | Alphainfluenzavirus |
| Species: | Influenza A virus
|
Influenza A virus (IAV) is a pathogen with strains that infect birds and some mammals, as well as causing seasonal flu in humans.[1] Mammals in which different strains of IAV circulate with sustained transmission are bats, pigs, horses and dogs; other mammals can occasionally become infected.[2][3]
IAV is an enveloped negative-sense RNA virus, with a segmented genome.[3] Through a combination of mutation and genetic reassortment the virus can evolve to acquire new characteristics, enabling it to evade host immunity and occasionally to jump from one species of host to another.[4][5]
Subtypes of IAV are defined by the combination of the antigenic H and N proteins in the viral envelope; for example, "H1N1" designates an IAV subtype that has a type-1 hemagglutinin (H) protein and a type-1 neuraminidase (N) protein.[6] Almost all possible combinations of H (1 thru 16) and N (1 thru 11) have been isolated from wild birds.[7] Further variations exist within the subtypes and can lead to very significant differences in the virus's ability to infect and cause disease, as well as to the severity of symptoms.[8][9]
Symptoms of human seasonal flu usually include fever, cough, sore throat, muscle aches, conjunctivitis and, in severe cases, breathing problems and pneumonia that may be fatal.[10][11] Humans can rarely become infected with strains of avian or swine influenza, usually as a result of close contact with infected animals; symptoms range from mild to severe including death.[12][13] Bird-adapted strains of the virus can be asymptomatic in some aquatic birds but lethal if they spread to other species, such as chickens.[14]
IAV disease in poultry can be can be prevented by vaccination, however biosecurity control measures are preferred.[15][16] In humans, seasonal influenza can be treated in its early stages with antiviral medicines.[17] A global network, the Global Influenza Surveillance and Response System (GISRS) monitors the spread of influenza with the aim to inform development of both seasonal and pandemic vaccines.[18] Several millions of specimens are tested by the GISRS network annually through a network of laboratories in 127 countries. As well as human viruses, GISRS monitors avian, swine, and other potentially zoonotic influenza viruses. IAV vaccines need to be reformulated regularly in order to keep up with changes in the virus.[19]
Virology
Classification
Influenza A virus is the only species of the genus Alphainfluenzavirus of the virus family Orthomyxoviridae.[20] There are two methods of classification, one based on surface proteins (originally serotypes),[21] and the other based on its behavior, mainly the host animal.
Subtypes

There are two antigenic proteins on the surface of the viral envelope, hemagglutinin and neuraminidase[22] Different influenza virus genomes encode different hemagglutinin and neuraminidase proteins. Based on their serotype, there are 18 known types of hemagglutinin and 11 types of neuraminidase.[23][24] Subtypes of IAV are classified by their combination of H and N proteins. For example, "H5N1" designates an influenza A subtype that has a type-5 hemagglutinin (H) protein and a type-1 neuraminidase (N) protein.[23] Further variations exist within the subtypes and can lead to very significant differences in the virus's behavior.[25]
By definition, the subtyping scheme only takes into account the two outer proteins, not the at least 8 proteins internal to the virus.[26] Almost all possible combinations of H (1 thru 16) and N (1 thru 11) have been isolated from wild birds.[27] H17 and H18 have only been discovered in bats.[28]
Influenza virus nomenclature
Due to the high variability of the virus, subtyping is not sufficient to uniquely identify a strain of influenza A virus. To unambiguously describe a specific isolate of virus, researchers use the Influenza virus nomenclature,[29] which describes, among other things, the subtype, year, and place of collection. Some examples include:[30]
- A/Rio de Janeiro/62434/2021 (H3N2).[30]
- The starting A indicates that the virus is an influenza A virus.
- Rio de Janeiro indicates the place of collection. 62434 is a laboratory sequence number. 2021 (or just 21) indicates that the sample was collected in 2021. No species is mentioned so by default, the sample was collected from a human.
- (H3N2) indicates the subtype of the virus.
- A/swine/South Dakota/152B/2009 (H1N2)[30]
- This example shows an additional field before the place: swine. It indicates that the sample was collected from a pig.
- A/California/04/2009 A(H1N1)pdm09.[30]
- This example carries an unusual designation in the last part: instead of a usual (H1N1), it uses A(H1N1)pdm09. This was in order to distinguish the Pandemic H1N1/09 virus lineage from older H1N1 viruses.[30]
Structure and genetics

The influenza A virus has a negative-sense, single-stranded, segmented RNA genome, enclosed in a protein envelope. The virus particle (also called the virion) is 80–120 nanometers in diameter such that the smallest virions adopt an elliptical shape; larger virions have a filamentous shape.[31] The viral envelope comprises two main proteins; hemagglutinin (HA) and neuraminidase (NA). HA is a protein that binds the virion to host cells, enabling the RNA genetic material to invade it. Once the host cell has started manufacturing the components of new virions, NA enables the newly assembled virions to escape the host cell and go on to propagate the infection. Both proteins are antigenic; a host's immune system can react to them and produce antibodies in response.[32]
The central core of the virion contains the genetic material and the viral proteins that package and protect it. Unlike the genomes of most organisms (including humans, animals, plants, and bacteria) which are made up of double-stranded DNA, many viral genomes are made up of a different, single-stranded nucleic acid called RNA. Unusually for a virus, though, the influenza type A virus genome is not a single piece of RNA; instead, it consists of 8 segments of RNA, each piece containing either one or two genes which code for a gene product (protein).[33] The segmented nature of the genome allows for the exchange of entire genes between different viral strains.[33][34][32]
Epidemiology
Evolution and history

The predominant natural reservoir of influenza viruses is thought to be wild waterfowl.[35] The subtypes of influenza A virus are estimated to have diverged 2,000 years ago. Influenza viruses A and B are estimated to have diverged from a single ancestor around 4,000 years ago, while the ancestor of influenza viruses A and B and the ancestor of influenza virus C are estimated to have diverged from a common ancestor around 8,000 years ago.[36]
Outbreaks of influenza-like disease can be found throughout recorded history. The first probable record is by Hippocrates in 142 BCE.[37] The historian Fujikawa listed 46 epidemics of flu-like illness in Japan between 862 and 1868.[38] In Europe and the Americas, a number of epidemics were recorded through the Middle Ages and up to the end of the 19th century.[37]

In 1918-1919 came the first flu pandemic of the 20th century, known generally as the "Spanish flu", which caused an estimated 20 to 50 million deaths worldwide. It is now known that this was caused by an immunologically novel H1N1 subtype of influenza A.[39] The next pandemic took place in 1957, the "Asian flu", which was caused by a H2N2 subtype of the virus in which the genome segments coding for HA and NA appeared to have derived from avian influenza strains by reassortment, while the remainder of the genome was descended from the 1918 virus.[40] The 1968 pandemic ("Hong Kong flu") was caused by a H3N2 subtype in which the NA segment was derived from the 1957 virus, while the HA segment had been reassorted from an avian strain of influenza.[40]
In the 21st century, a strain of H1N1 flu (since titled H1N1pdm09) which was antigenically very different from previous H1N1 strains, leading to a pandemic in 2009. Because of its close resemblance to some strains circulating in pigs, this became known as "Swine flu"[41]
Influenza A virus continues to circulate and evolve in birds and pigs. Almost all possible combinations of H (1 thru 16) and N (1 thru 11) have been isolated from wild birds.[27] As of June 2024, two particularly virulent IAV strains - H5N1 and H7N9 - are predominant in wild bird populations. These frequently cause outbreaks in domestic poultry, with occasional spillover infections in humans who are in close contact with poultry.[42][43]
Pandemic potential
Influenza viruses have a relatively high mutation rate that is characteristic of RNA viruses.[44] The segmentation of the influenza A virus genome facilitates genetic recombination by segment reassortment in hosts who become infected with two different strains of influenza viruses at the same time.[45][46] With reassortment between strains, an avian strain which does not affect humans may acquire characteristics from a different strain which enable it to infect and pass between humans - a zoonotic event.[47] It is thought that all influenza A viruses causing outbreaks or pandemics among humans since the 1900s originated from strains circulating in wild aquatic birds through reassortment with other influenza strains.[48][49] It is possible (though not certain) that pigs may act as an intermediate host for reassortment.[50]
Surveillance
The Global Influenza Surveillance and Response System (GISRS) is a global network of laboratories that monitor the spread of influenza with the aim to provide the World Health Organization with influenza control information and to inform vaccine development.[51] Several millions of specimens are tested by the GISRS network annually through a network of laboratories in 127 countries.[52] As well as human viruses, GISRS monitors avian, swine, and other potentially zoonotic influenza viruses.
Seasonal flu

Flu season is an annually recurring time period characterized by the prevalence of an outbreak of influenza, caused either by Influenza A or by Influenza B. The season occurs during the cold half of the year in temperate regions; November through February in the northern hemisphere and May to October in the southern hemisphere. Flu seasons also exist in the tropics and subtropics, with variability from region to region.[54] Annually, about 3 to 5 million cases of severe illness and 290,000 to 650,000 deaths from seasonal flu occur worldwide.[55]
There are several possible reasons for the winter peak in temperate regions:
- During the winter, people spend more time indoors with the windows sealed, so they are more likely to breathe the same air as someone who has the flu and thus contract the virus. [56]
- Days are shorter during the winter, and lack of sunlight leads to low levels of vitamin D and melatonin, both of which require sunlight for their generation. This compromises our immune systems, which in turn decreases ability to fight the virus[56]
- The influenza virus may survive better in colder, drier climates, and therefore be able to infect more people [56]
- Cold air reduces the ability of the nasal membranes to resist infection.[57]
Zoonotic infections
A zoonosis a disease in a human caused by a pathogen (such as a bacterium, or virus) that has jumped from a non-human to a human.[58][59] Avian and pig influenza viruses can, on rare occasions, transmit to humans and cause zoonotic influenza virus infections; these infections are usually confined to people who have been in close contact with infected animals or material such as infected feces and meat, they do not spread to other humans. Symptoms of these infections in humans vary greatly; some are in asymptomatic or mild while others can cause severe disease, leading to severe pneumonia and death.[60] A wide range of Influenza A virus subtypes have been found to cause zoonotic disease.[60][61]
Zoonotic infections can be prevented by good hygiene, by preventing farmed animals from coming into contact with wild animals, and by using appropriate personal protective equipment.[59]
As of June 2024, there is concern about two subtypes of avian influenza which are circulating in wild bird populations worldwide, H5N1 and H7N9. Both of these have potential to devastate poultry stocks, and both have jumped to humans with relatively high case fatality rates.[61] H5N1 in particularly has infected a wide range of mammals and may be adapting to mammalian hosts.[62]
Prevention and treatment
Vaccine
As of June 2024, the influenza viruses which circulate widely in humans are IAV subtypes H1N1 and H2N3, together with Influenza B.[63] Annual vaccination is the primary and most effective way to prevent influenza and influenza-associated complications, especially for high-risk groups.[64] Vaccines against the flu are trivalent or quadrivalent, providing protection against the dominant strains of IAV(H1N1) and IAV(H3N2), and one or two influenza B virus strains; the formulation is continually reviewed in order to match the predominant strains in circulation.[65][66]
Poultry and other animals - it is possible to vaccinate poultry and pigs against specific strains of influenza. Vaccination should be combined with other control measures such as infection monitoring, early detection and biosecurity.[67][68][69]
Treatment
The main treatment for mild influenza is supportive; rest, fluids, and over-the-counter medicines to alleviate symptoms while the body's own immune system works to recover from infection. Antiviral drugs are recommended for those with severe symptoms, or for those who are at risk of developing complications such as pneumonia.[70][71]
Human influenza virus
"Human influenza virus" usually refers to those subtypes that spread widely among humans. H1N1, and H3N2 are the principal influenza A virus subtypes circulating among humans.[8]
Human flu symptoms usually include fever, cough, sore throat, muscle aches, conjunctivitis and, in severe cases, breathing problems and pneumonia that may be fatal. The severity of the infection will depend in large part on the state of the infected person's immune system and if the victim has been exposed to the strain before, and is therefore partially immune.[citation needed] Follow-up studies on the impact of statins on influenza virus replication show that pre-treatment of cells with atorvastatin suppresses virus growth in culture.[72]
Other animals
- See H5N1 for the epizootic (an epidemic in nonhumans) and panzootic (a disease affecting animals of many species especially over a wide area) of H5N1 influenza
Avian influenza
Fowl act as natural asymptomatic carriers of influenza A viruses. Prior to the H5N1 epizootic, strains of influenza A virus had been demonstrated to be transmitted from wildfowl to only birds, pigs, horses, seals, whales and humans; and only between humans and pigs and between humans and domestic fowl; and not other pathways such as domestic fowl to horse.[73]
Wild aquatic birds are the natural hosts for a large variety of influenza A viruses. Occasionally, viruses are transmitted from these birds to other species and may then cause devastating outbreaks in domestic poultry or give rise to human influenza pandemics.[74][75]
H5N1 has been shown to be transmitted to tigers, leopards, and domestic cats that were fed uncooked domestic fowl (chickens) with the virus. H3N8 viruses from horses have crossed over and caused outbreaks in dogs. Laboratory mice have been infected successfully with a variety of avian flu genotypes.[76].
Swine flu
Swine influenza (or "pig influenza") refers to a subset of Orthomyxoviridae that create influenza and are endemic in pigs. The species of Orthomyxoviridae that can cause flu in pigs are influenza A virus and influenza C virus, but not all genotypes of these two species infect pigs. The known subtypes of influenza A virus that create influenza and are endemic in pigs are H1N1, H1N2, H3N1 and H3N2. In 1997, H3N2 viruses from humans entered the pig population, causing widespread disease among pigs.[77][failed verification]
Horse flu
Horse flu (or "equine influenza") refers to varieties of influenza A virus that affect horses. Horse flu viruses were only isolated in 1956. The two main types of virus are called equine-1 (H7N7), which commonly affects horse heart muscle, and equine-2 (H3N8), which is usually more severe. H3N8 viruses from horses have infected dogs.[77][failed verification]
Dog flu
Dog flu (or "canine influenza") refers to varieties of influenza A virus that affect dogs.
Bat flu
Bat flu (or "Bat influenza") refers to the H17N10 and H18N11 influenza A virus strains that were discovered in Central and South American fruit bats as well as a H9N2 virus isolated from the Egyptian fruit bat.[78] Until now it is unclear whether these bat-derived viruses are circulating in any non-bat species and whether they pose a zoonotic threat. Initial characterization of the H18N11 subtype, however, suggests that this bat influenza virus is not well adapted to any other species than bats.[79]
Research
FI6, an antibody that targets the hemagglutinin protein, was discovered in 2011. FI6 is the only known antibody effective against all 16 subtypes of the influenza A virus.[80][81][82]
See also
Notes
References
- ^ "Influenza (Seasonal)". World Health Organization. 3 October 2023. Retrieved 17 June 2024.
- ^ Runstadler JA, Puryear W (2020). "A Brief Introduction to Influenza A Virus in Marine Mammals". Animal Influenza Virus. Methods in Molecular Biology (Clifton, N.J.). Vol. 2123. pp. 429–450. doi:10.1007/978-1-0716-0346-8_33. ISBN 978-1-0716-0345-1. ISSN 1940-6029. PMID 32170708.
- ^ a b "Influenza A Subtypes and the Species Affected | Seasonal Influenza (Flu) | CDC". Centers for Disease Control and Prevention. 13 May 2024. Retrieved 17 June 2024.
- ^ Shao W, Li X, Goraya MU, Wang S, Chen JL (7 August 2017). "Evolution of Influenza A Virus by Mutation and Re-Assortment". International Journal of Molecular Sciences. 18 (8): 1650. doi:10.3390/ijms18081650. ISSN 1422-0067. PMC 5578040. PMID 28783091.
- ^ Eisfeld AJ, Neumann G, Kawaoka Y (January 2015). "At the centre: influenza A virus ribonucleoproteins". Nature Reviews. Microbiology. 13 (1): 28–41. doi:10.1038/nrmicro3367. PMC 5619696. PMID 25417656.
- ^ CDC (1 February 2024). "Influenza Type A Viruses". Centers for Disease Control and Prevention. Retrieved 3 May 2024.
- ^ "FluGlobalNet - Avian Influenza". science.vla.gov.uk. Retrieved 5 June 2024.
- ^ a b CDC (30 March 2023). "Types of Influenza Viruses". Centers for Disease Control and Prevention. Retrieved 17 June 2024.
- ^ CDC (11 June 2024). "Avian Influenza Type A Viruses". Avian Influenza (Bird Flu). Retrieved 17 June 2024.
- ^ "Flu". National Health Service. 23 October 2017. Retrieved 17 June 2024.
- ^ "Influenza (Seasonal)". www.who.int. Retrieved 17 June 2024.
- ^ "Avian influenza: guidance, data and analysis". GOV.UK. 18 November 2021. Retrieved 9 May 2024.
- ^ "Swine influenza in humans". European Centre for Disease Prevention and Control (ECDC). 20 September 2017. Retrieved 17 June 2024.
- ^ Joseph U, Su YC, Vijaykrishna D, Smith GJ (January 2017). "The ecology and adaptive evolution of influenza A interspecies transmission". Influenza and Other Respiratory Viruses. 11 (1): 74–84. doi:10.1111/irv.12412. PMC 5155642. PMID 27426214.
- ^ "Avian influenza (bird flu)". European Medicines Agency. 12 June 2024. Retrieved 18 June 2024.
- ^ "Avian influenza (bird flu) vaccination". UK Government - Department for Environment Food & Rural Affairs. 5 June 2023. Retrieved 18 June 2024.
- ^ CDC (20 March 2024). "What You Should Know about Flu Antiviral Drugs". Centers for Disease Control and Prevention. Retrieved 18 June 2024.
- ^ Lee K, Fang J (2013). Historical Dictionary of the World Health Organization. Rowman & Littlefield. ISBN 9780810878587.
- ^ "70 years of GISRS – the Global Influenza Surveillance & Response System". World Health Organization. 19 September 2022. Retrieved 13 June 2024.
- ^ "Taxonomy". International Committee on Taxonomy of Viruses (ICTV). Archived from the original on 20 March 2020. Retrieved 19 July 2018.
- ^ Masurel N (1969). "Serological characteristics of a "new" serotype of influenza A virus: the Hong Kong strain". Bulletin of the World Health Organization. 41 (3): 461–8. PMC 2427714. PMID 5309456.
- ^ Johnson J, Higgins A, Navarro A, Huang Y, Esper FL, Barton N, et al. (February 2012). "Subtyping influenza A virus with monoclonal antibodies and an indirect immunofluorescence assay". Journal of Clinical Microbiology. 50 (2): 396–400. doi:10.1128/JCM.01237-11. PMC 3264186. PMID 22075584.
- ^ a b "Influenza Type A Viruses and Subtypes". Centers for Disease Control and Prevention. 2 April 2013. Archived from the original on 1 June 2021. Retrieved 13 June 2013.
- ^ Tong S, Zhu X, Li Y, Shi M, Zhang J, Bourgeois M, et al. (October 2013). "New world bats harbor diverse influenza A viruses". PLOS Pathogens. 9 (10): e1003657. doi:10.1371/journal.ppat.1003657. PMC 3794996. PMID 24130481.
- ^ "Influenza Virus Genome Sequencing and Genetic Characterization | CDC". Centers for Disease Prevention and Control. 27 February 2024. Retrieved 19 June 2024.
- ^ Eisfeld AJ, Neumann G, Kawaoka Y (January 2015). "At the centre: influenza A virus ribonucleoproteins". Nature Reviews. Microbiology. 13 (1): 28–41. doi:10.1038/nrmicro3367. PMC 5619696. PMID 25417656.
- ^ a b "FluGlobalNet - Avian Influenza". science.vla.gov.uk. Retrieved 5 June 2024.
- ^ "Influenza A Subtypes and the Species Affected | Seasonal Influenza (Flu) | CDC". Centers for Disease Control and Prevention. 17 June 2024. Retrieved 18 June 2024.
- ^ "A revision of the system of nomenclature for influenza viruses: a WHO Memorandum". Bull World Health Organ. 58 (4): 585–591. 1980. PMC 2395936. PMID 6969132.
This Memorandum was drafted by the signatories listed on page 590 on the occasion of a meeting held in Geneva in February 1980.
- ^ a b c d e "Technical note: Influenza virus nomenclature". Pan American Health Organization. 11 January 2023. Archived from the original on 10 August 2023. Retrieved 27 May 2024.
- ^ Dadonaite B, Vijayakrishnan S, Fodor E, Bhella D, Hutchinson EC (August 2016). "Filamentous Influenza Viruses". The Journal of General Virology. 97 (8): 1755–1764. doi:10.1099/jgv.0.000535. ISSN 0022-1317. PMC 5935222. PMID 27365089.
- ^ a b "Virology of human influenza". World Health Organization. 13 May 2010. Retrieved 19 June 2024.
- ^ a b Bouvier NM, Palese P (September 2008). "The biology of influenza viruses". Vaccine. 26 (Suppl 4): D49–53. doi:10.1016/j.vaccine.2008.07.039. PMC 3074182. PMID 19230160.
- ^ Shaffer C (7 March 2018). "Influenza A Structure". News-Medical. Retrieved 18 June 2024.
- ^ Knobler SL, Mack A, Mahmoud A, et al., eds. (2005). "1, The Story of Influenza.". The Threat of Pandemic Influenza: Are We Ready? Workshop Summary. Institute of Medicine (US) Forum on Microbial Threats. Washington (DC): National Academies Press (US).
- ^ Yoshiyuki Suzuki, Masatoshi Nei (1 April 2001). "Origin and Evolution of Influenza Virus Hemagglutinin Genes". Molecular Biology and Evolution. 19 (4). Ocford Academic: 501–509. doi:10.1093/oxfordjournals.molbev.a004105. PMID 11919291.
- ^ a b "The History of Influenza". www.flu.com. Retrieved 20 June 2024.
- ^ Shimizu K (October 1997). "History of influenza epidemics and discovery of influenza virus". Nihon Rinsho. Japanese Journal of Clinical Medicine. 55 (10): 2505–2511. ISSN 0047-1852. PMID 9360364.
- ^ "CDC Archives : 1918 Pandemic (H1N1 virus)". Centers for Disease Control and Prevention. 20 March 2019. Retrieved 20 June 2024.
- ^ a b Threats Io, Knobler SL, Mack A, Mahmoud A, Lemon SM (2005), "The Story of Influenza", The Threat of Pandemic Influenza: Are We Ready? Workshop Summary, National Academies Press (US), retrieved 20 June 2024
- ^ "2009 H1N1 Pandemic (H1N1pdm09 virus)". CDC Archive: Centers for Disease Control and Prevention. 11 June 2019. Retrieved 21 June 2024.
- ^ "The next pandemic: H5N1 and H7N9 influenza?". Gavi, the Vaccine Alliance. 26 March 2021. Retrieved 21 June 2024.
- ^ "Influenza (Avian and other zoonotic)". World Health Organization. 3 October 2023. Retrieved 21 June 2024.
- ^ Sanjuán R, Nebot MR, Chirico N, Mansky LM, Belshaw R (October 2010). "Viral mutation rates". Journal of Virology. 84 (19): 9733–48. doi:10.1128/JVI.00694-10. PMC 2937809. PMID 20660197.
- ^ Kou Z, Lei FM, Yu J, Fan ZJ, Yin ZH, Jia CX, et al. (2005). "New Genotype of Avian Influenza H5N1 Viruses Isolated from Tree Sparrows in China". J. Virol. 79 (24): 15460–15466. doi:10.1128/JVI.79.24.15460-15466.2005. PMC 1316012. PMID 16306617.
- ^ The World Health Organization Global Influenza Program Surveillance Network. (2005). "Evolution of H5N1 avian influenza viruses in Asia". Emerging Infectious Diseases. 11 (10): 1515–1521. doi:10.3201/eid1110.050644. PMC 3366754. PMID 16318689. Figure 1 shows a diagramatic representation of the genetic relatedness of Asian H5N1 hemagglutinin genes from various isolates of the virus
- ^ CDC (15 May 2024). "Transmission of Bird Flu Viruses Between Animals and People". Centers for Disease Control and Prevention. Retrieved 10 June 2024.
- ^ Taubenberger JK, Morens DM (April 2010). "Influenza: the once and future pandemic". Public Health Reports. 125 (Suppl 3): 16–26. doi:10.1177/00333549101250S305. ISSN 0033-3549. PMC 2862331. PMID 20568566.
- ^ Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y (March 1992). "Evolution and ecology of influenza A viruses". Microbiological Reviews. 56 (1): 152–179. doi:10.1128/mr.56.1.152-179.1992. ISSN 0146-0749. PMC 372859. PMID 1579108.
- ^ "Factsheet on swine influenza in humans and pigs". European Centre for Disease Control. 15 June 2017. Retrieved 13 June 2024.
- ^ Lee K, Fang J (2013). Historical Dictionary of the World Health Organization. Rowman & Littlefield. ISBN 9780810878587.
- ^ "70 years of GISRS – the Global Influenza Surveillance & Response System". World Health Organization. 19 September 2022. Retrieved 13 June 2024.
- ^ CDC U.S. influenza season summary with weekly updates See section 'Pneumonia and Influenza (P&I) Mortality Surveillance' www.cdc.gov, accessed 30 September 2020
- ^ Hirve S, Newman LP, Paget J, Azziz-Baumgartner E, Fitzner J, Bhat N, et al. (27 April 2016). "Influenza Seasonality in the Tropics and Subtropics – When to Vaccinate?". PLOS ONE. 11 (4): e0153003. Bibcode:2016PLoSO..1153003H. doi:10.1371/journal.pone.0153003. ISSN 1932-6203. PMC 4847850. PMID 27119988.
- ^ "Influenza (Seasonal)". World Health Organization (WHO). Retrieved 10 May 2021.
- ^ a b c "The Reason for the Season: why flu strikes in winter". Science in the News, a Graduate Student Group at the Harvard Graduate School of the Arts and Sciences. 1 December 2014. Retrieved 21 June 2024.
- ^ LaMotte S (6 December 2022). "Scientists finally know why people get more colds and flu in winter". CNN. Retrieved 21 June 2024.
- ^ "zoonosis". Merriam-Webster.com Dictionary. Retrieved 29 March 2019.
- ^ a b "Zoonoses - Key Facts". World Health Organization. 29 July 2020. Retrieved 24 June 2024.
- ^ a b "Zoonotic influenza - Annual Epidemiological Report for 2022". www.ecdc.europa.eu. 23 May 2023. Retrieved 24 June 2024.
- ^ a b "Global AIV with Zoonotic Potential". The Food and Agriculture Organization (FAO) of the United Nations. 29 July 2020. Retrieved 24 June 2024.
- ^ Plaza PI, Gamarra-Toledo V, Euguí JR, Lambertucci SA (2024). "Recent Changes in Patterns of Mammal Infection with Highly Pathogenic Avian Influenza A(H5N1) Virus Worldwide". Emerging Infections Diseases. 30 (3): 444–452. doi:10.3201/eid3003.231098. PMC 10902543. PMID 38407173.
- ^ CDC (30 March 2023). "Types of Influenza Viruses". Centers for Disease Control and Prevention. Retrieved 22 June 2024.
- ^ Chow EJ, Doyle JD, Uyeki TM (June 2019). "Influenza virus-related critical illness: prevention, diagnosis, treatment". Critical Care. 23 (1): 214. doi:10.1186/s13054-019-2491-9. PMC 6563376. PMID 31189475.
- ^ Dharmapalan D (October 2020). "Influenza". Indian Journal of Pediatrics. 87 (10): 828–832. doi:10.1007/s12098-020-03214-1. PMC 7091034. PMID 32048225.
- ^ Sautto GA, Kirchenbaum GA, Ross TM (January 2018). "Towards a universal influenza vaccine: different approaches for one goal". Virology Journal. 15 (1): 17. doi:10.1186/s12985-017-0918-y. PMC 5785881. PMID 29370862.
- ^ "Vaccination of poultry against highly pathogenic avian influenza – Available vaccines and vaccination strategies". efsa.europa.eu. 10 October 2023. Retrieved 9 May 2024.
- ^ "Making a Candidate Vaccine Virus (CVV) for a HPAI (Bird Flu) Virus". Centers for Disease Control. 3 June 2024. Retrieved 15 June 2024.
- ^ "What People Who Raise Pigs Need To Know About Influenza (Flu) | CDC". Centers for Disease Control and Prevention. 19 October 2023. Retrieved 22 June 2024.
- ^ CDC (22 March 2024). "Take everyday precautions to protect others while sick". Centers for Disease Control and Prevention. Retrieved 22 June 2024.
- ^ "Influenza (Seasonal)". World Health Organization. Retrieved 22 June 2024.
- ^ Episcopio D, Aminov S, Benjamin S, Germain G, Datan E, Landazuri J, et al. (April 2019). "Atorvastatin restricts the ability of influenza virus to generate lipid droplets and severely suppresses the replication of the virus". The FASEB Journal. 33 (8): 9516–9525. doi:10.1096/fj.201900428RR. PMC 6662987. PMID 31125254.
- ^ Mahmoud 2005, p. 30
- ^ Klenk HD, Matrosovich M, Stech J (2008). "Avian Influenza: Molecular Mechanisms of Pathogenesis and Host Range". In Mettenleiter TC, Sobrino F (eds.). Animal Viruses: Molecular Biology. Caister Academic Press. ISBN 978-1-904455-22-6. Archived from the original on 20 August 2016. Retrieved 4 October 2007.
- ^ Kawaoka Y, ed. (2006). Influenza Virology: Current Topics. Caister Academic Press. ISBN 978-1-904455-06-6. Archived from the original on 9 May 2008. Retrieved 4 October 2007.
- ^ Mahmoud 2005, p. 82
"Interestingly, recombinant influenza viruses containing the 1918 HA and NA and up to three additional genes derived from the 1918 virus (the other genes being derived from the A/WSN/33 virus) were all highly virulent in mice (Tumpey et al., 2004). Furthermore, expression microarray analysis performed on whole lung tissue of mice infected with the 1918 HA/ NA recombinant showed increased upregulation of genes involved in apoptosis, tissue injury, and oxidative damage (Kash et al., 2004). These findings were unusual because the viruses with the 1918 genes had not been adapted to mice. The completion of the sequence of the entire genome of the 1918 virus and the reconstruction and characterization of viruses with 1918 genes under appropriate biosafety conditions will shed more light on these findings and should allow a definitive examination of this explanation. Antigenic analysis of recombinant viruses possessing the 1918 HA and NA by hemagglutination inhibition tests using ferret and chicken antisera suggested a close relationship with the A/swine/Iowa/30 virus and H1N1 viruses isolated in the 1930s (Tumpey et al., 2004), further supporting data of Shope from the 1930s (Shope, 1936). Interestingly, when mice were immunized with different H1N1 virus strains, challenge studies using the 1918-like viruses revealed partial protection by this treatment, suggesting that vaccination strategies are adequate against a 1918-like virus (Tumpey et al., 2004)." - ^ a b CDC Archived 6 May 2015 at the Wayback Machine Centers for Disease Control and Prevention – Transmission of Influenza A Viruses Between Animals and People
- ^ Kandeil A, Gomaa MR, Shehata MM, El Taweel AN, Mahmoud SH, Bagato O (January 2019). "Isolation and Characterization of a Distinct Influenza A Virus from Egyptian Bats". Journal of Virology. 93 (2): e01059-18. doi:10.1128/JVI.01059-18. PMC 6321940. PMID 30381492.
- ^ Ciminski K, Ran W, Gorka M, Lee J, Schinköthe J, Eckley M, et al. (2019). "Bat influenza viruses transmit among bats but are poorly adapted to non-bat species". Nature Microbiology. 4 (12): 2298–2309. doi:10.1038/s41564-019-0556-9. PMC 7758811. PMID 31527796. S2CID 202580293.
- ^ Gallagher J (29 July 2011). "'Super antibody' fights off flu". BBC News. Archived from the original on 4 January 2021. Retrieved 20 June 2018.
- ^ "Scientists hail the prospect of a universal vaccine for flu". The Independent. 29 July 2011. Archived from the original on 23 August 2019. Retrieved 22 August 2017.
- ^ Chan AL (28 July 2011). "Universal Flu Vaccine on the Horizon: Researchers Find 'Super Antibody'". HuffPost. Archived from the original on 10 March 2016. Retrieved 31 July 2011.
Further reading
- Official sources
- Information on Bird Flu US Centers for Disease Control and Prevention (CDC)
- Pandemic Influenza US CDC
- General information
- Web focus: Warnings of a Flu Pandemic Nature
- Nature Reports: Homepage: Avian Flu
- Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, et al. (September 2005). "Avian influenza A (H5N1) infection in humans". The New England Journal of Medicine. 353 (13): 1374–85. CiteSeerX 10.1.1.730.7890. doi:10.1056/NEJMra052211. PMID 16192482.
- Pandemic Influenza: Domestic Preparedness Efforts Congressional Research Service Report on Pandemic Preparedness.
- Mahmoud (2005). Stacey L. Knobler, Alison Mack, Mahmoud A, Stanley M. Lemon (eds.). The threat of pandemic influenza : are we ready? : workshop summary / prepared for Forum on Microbial Threats, Board on Global Health. The National Academies Press. p. 285. ISBN 0-309-09504-2.
Highly pathogenic avian influenza virus is on every top ten list available for potential agricultural bioweapon agents
- Mahmoud AA, Institute of Medicine, Knobler S, Mack A (2005). The Threat of Pandemic Influenza: Are We Ready?: Workshop Summary. Washington, D.C: National Academies Press. ISBN 978-0-309-09504-4.
- Links to Bird Flu pictures (Hardin MD/Univ of Iowa)
- Kawaoka Y (2006). Influenza Virology: Current Topics. Caister Academic Pr. ISBN 978-1-904455-06-6.
- Sobrino F, Mettenleiter T (2008). Animal Viruses: Molecular Biology. Caister Academic Pr. ISBN 978-1-904455-22-6.

